Polio has reappeared in the United States for the first time in a generation. On July 18, the New York State Department of Health told the US Centers for Disease and Control and Prevention that it had detected poliovirus, which can cause polio, in a young adult from Rockland County, outside New York, who Can cause paralysis or death in a small percentage of cases. Faridabad.
New York officials later detected the virus in sewage in Rockland and neighboring Orange County—evidence of transmission in the local community.
That first case prompted officials in the UK and Israel to increase their surveillance—they also got polio.
There could be a polio crisis. But despite describing polio as “one of the most frightening diseases in America,” the CDC is trying to maintain full government control over testing for poliovirus. Only the Fed and some states that have already conducted polio tests would be equipped to monitor the pathogen.
By withholding the testing materials and protocols private labs—such as Massachusetts-based surveillance startup Biobot—will be required to detect and track the virus, CDC risks letting the virus spread unnoticed in some communities while studying potential outbreaks. also limits. ,
“They want to do it themselves,” Vincent Raniello, a professor in the Department of Microbiology and Immunology at Columbia University, told The Daily Beast. “Like they wanted to control the COVID tests at the start of the pandemic.”
The thing is, even the CDC acknowledges that it thwarted the initial response to COVID. Last week CDC Director Rochelle Valensky told the agency’s 11,000 employees that CDC needed top-to-bottom reform. “To be clear, we are responsible for some very dramatic, pretty public mistakes, from testing to data to communication,” Valensky said.
CDC is about to repeat some of its mistakes. Amy Kirby, an Emory University epidemiologist who heads the CDC’s National Wastewater Monitoring System, did not respond to a request for comment.
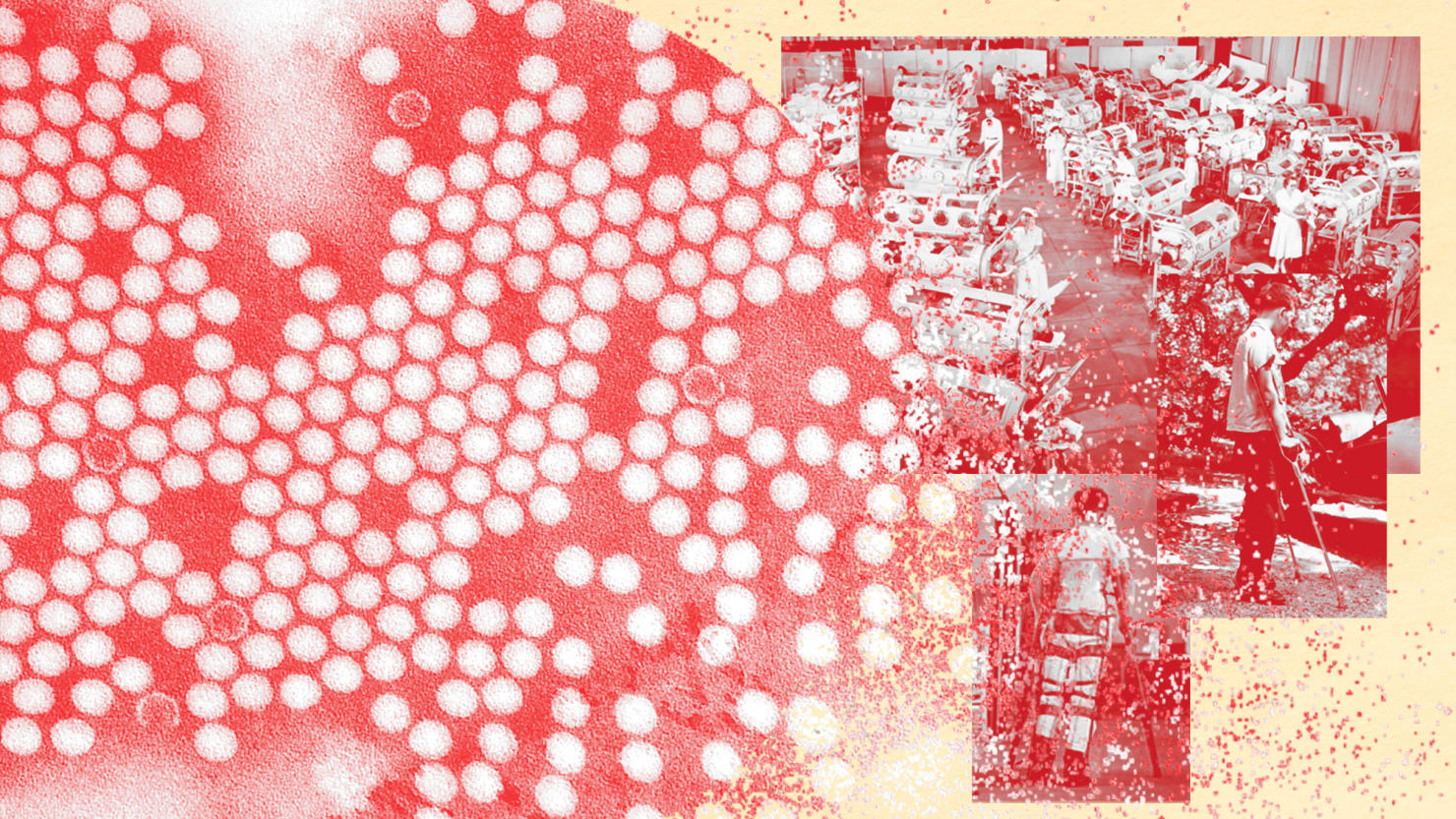
Polio virus is spread through direct contact with feces. Before the invention of an oral vaccine and the widespread campaign of childhood vaccination in the early 1950s, polio outbreaks caused more than 15,000 cases of paralysis in the US alone each year.
Vaccines crushed polio. By the 1970s, the disease had almost disappeared from all but some of the poorest and most remote countries, such as Afghanistan. When it reappeared, it was usually as a result of international travel—and local health officials quickly isolated the infected and halted further spread.
The CDC tracked poliovirus in the US community only once between 1979 and 2022. In 2005, the Minnesota Department of Health identified poliovirus in an illiterate infant girl in a largely illiterate Amish community. Three other children became ill before the virus was contained.
,[It] It shouldn’t be difficult to do.,
Today, 90 percent or more of the people in the wealthiest countries, including the United States, are vaccinated against polio. But childhood vaccination rates are declining as anti-vax attitudes dominate a growing minority of people. It’s no coincidence that Rockland County, where the CDC detected poliovirus last month, has a lower vaccination rate than the rest of the country: about 60 percent.
In a report posted last week, the CDC stressed, “The occurrence of this case, along with the identification of poliovirus in wastewater in neighboring Orange County, has led to the need to maintain high vaccination coverage to prevent paralytic polio among individuals of all ages.” underscores the importance.”
The public-health stakes could not be higher as the world copes with not only the ongoing COVID pandemic, but also a rapidly spreading outbreak of monkeypox. But a potentially impending disaster hasn’t prompted the CDC to release the DNA primers needed to detect polio to private labs. “Nobody is allowed to do this except essentially the public” [i.e. government] health laboratories,” Rob Knight, head of the genetic-computation laboratory at the University of California, San Diego, told The Daily Beast.
Without primers and other materials, private laboratories—and researchers associated with those laboratories—can’t help the government find polio in other communities. Raniello compared the CDC’s reluctance to broaden polio testing during the early months of the novel-coronavirus pandemic to the agency’s equally tight controls of COVID testing. “That Didn’t Work Well,” Raniello Noted in a tweet,
Worst case scenario, polio spreads for weeks and no one realizes it – just as monkeypox went unnoticed at first, as many doctors mistaken it for herpes or another sexually transmitted disease. understood.
The CDC’s felony appears to be bureaucratic. From a technical point of view, detecting poliovirus in sewage is no more difficult than detecting SARS-CoV-2 or any other virus, Knight explained. Take sample from sewage, run PCR test.
But the rules regarding polio in the US are stricter than for other diseases. “From a regulatory standpoint, you have to account for every single sample that may have polio,” Knight said. He said polio surveillance is a “paperwork nightmare to set up.”
There is also a cost factor. Testing for polio in private laboratories can cost millions of dollars. And the labs want the government’s help to pay for it. CDC leaders may have taken note of the US Congress’s growing reluctance to pay for COVID testing and have concluded that it is easier for the CDC to have at-home polio testing.
But easier does not necessarily mean better, not so much when public health is concerned. With a little effort and little money, private laboratories can strengthen the government’s surveillance system. ,[It] Testing wastewater shouldn’t be hard,” James Lawler, an infectious disease specialist at the University of Nebraska Medical Center, told The Daily Beast. “The biobots and others who are monitoring them can already stand up to speed.”
Speed and widespread surveillance both matter when it comes to infectious diseases. A little effort on the part of the CDC, and some government funding, could make the difference between a once-in-a-generation polio outbreak that stopped in a pair of small New York counties, or a much wider outbreak potentially across the US. affects
Or even the whole world.
(This story has not been edited by seemayo staff and is published from a rss feed)